For decades, the war on cancer has been fought on the battleground of genetics, with billions poured into decoding DNA mutations. Yet survival rates for aggressive cancers like pancreatic cancer remain stubbornly low, and cases are skyrocketing—even among children as young as 8. Dr. Patrick Soon-Shiong, a surgeon with over 50 years of cancer research under his belt, is challenging the status quo with a bold claim: cancer isn’t primarily a genetic disease. Instead, he argues, it’s a failure of the immune system—a revelation that could reshape how we prevent and fight this devastating illness.
Soon-Shiong’s observations are alarming. He’s seeing pancreatic cancer in 13-year-olds, while colleagues report colon cancer in children as young as 8 to 11. Young adults are grappling with aggressive, “turbo-charged” cancers that progress at unprecedented rates. The traditional view—that cancer stems from random genetic mutations—isn’t holding up. Despite advances in genomics, the 5-year survival rate for pancreatic cancer lingers around 12%, per the American Cancer Society. “We’ve been missing something crucial,” Soon-Shiong says. His research points to a deeper culprit: a compromised immune system that fails to eliminate abnormal cells.
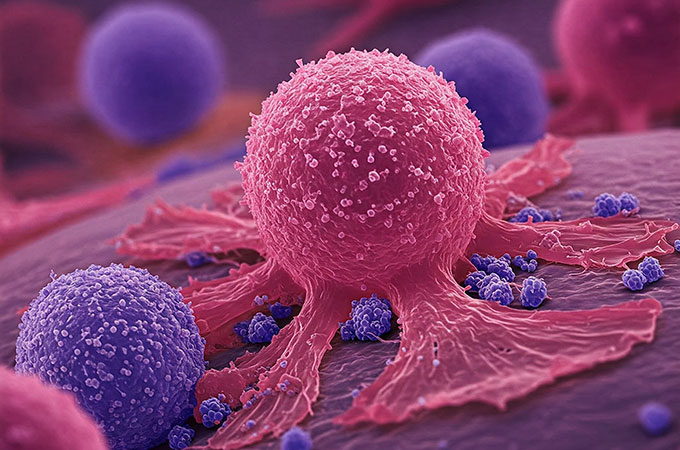
Our bodies are constantly producing potentially cancerous cells through normal cell division errors. Evolution equipped us with a defense system—natural killer (NK) cells and T-cells, which Soon-Shiong calls our “internal first responders.” These immune cells, discovered as recently as the 1970s, patrol the body, identifying and destroying threats. They maintain a delicate balance: “killer” cells attack abnormal cells, while “suppressor” cells prevent overreactions that could lead to autoimmune diseases. Cancer gains a foothold when this balance tips—when cancer cells either hide from killer cells or activate suppressor cells to shut down the immune response, allowing unchecked growth.
This immune-centric view explains why people with identical cancer mutations can have vastly different outcomes. The difference often lies in immune function and metabolic health. A key marker, often overlooked, is the Absolute Lymphocyte Count (ALC). Studies in journals like The Lancet Oncology show that low lymphocyte counts predict poorer outcomes across all cancer types, yet most oncologists don’t routinely monitor this metric. Adding to the challenge, standard treatments like chemotherapy and radiation—while shrinking tumors—deplete lymphocytes and damage NK cells, creating a paradox. “We’re winning the immediate battle but losing the long-term war,” Soon-Shiong warns.
What throws the immune system off balance in the first place? Chronic inflammation is a major driver, often fueled by processed foods, environmental toxins, viral infections, chronic stress, and poor sleep. These factors disrupt the harmony between killer and suppressor cells, paving the way for cancer. Sleep, for instance, is critical for NK cell regeneration, while specific wavelengths of sunlight can activate immune cells, per research in Nature Immunology. Soon-Shiong also points to metabolic health: “Cancer doesn’t develop in a body with healthy mitochondria and functioning immunity.”
His findings challenge another long-held belief—that cancers are distinct based on their location, like lung or breast cancer. Soon-Shiong’s tumor studies reveal that cancers from different organs often share identical molecular signatures at the protein level, not just the genetic level. “The gene doesn’t dictate treatment—the activated protein does,” he explains. This insight suggests a drug for breast cancer might work for colon cancer, a paradigm shift that could streamline treatment approaches.
So, what can we do? Soon-Shiong advocates for evidence-based strategies to bolster immunity: prioritize quality sleep, get regular sun exposure, and cut back on inflammatory foods and chemicals. Additional research supports time-restricted eating, strategic exercise, stress reduction, and minimizing exposure to toxins—all of which support metabolic and immune health. While these steps aren’t a cure, they could lower risk by keeping the body’s defenses sharp.
Soon-Shiong’s work is a wake-up call. Cancer’s rise, especially in the young, demands a new perspective—one that looks beyond genetics to the immune system’s critical role. As research evolves, his insights may pave the way for more effective prevention and treatment, giving hope to millions. But for now, the message is clear: protecting your immune system might be your best weapon in the fight against cancer.
This article is based on insights shared by Dr. Patrick Soon-Shiong in a post by Karl Mehta on X (https://x.com/karlmehta/status/1916115158591766652). Additional context was drawn from studies in The Lancet Oncology and Nature Immunology, as well as cancer statistics from the American Cancer Society. Special thanks to Karl Mehta for bringing Dr. Soon-Shiong’s groundbreaking perspective to light.

Thanks for your useful post. In recent times, I have come to be able to understand that the particular symptoms of mesothelioma cancer are caused by the build up of fluid between your lining in the lung and the breasts cavity. The condition may start in the chest area and get distributed to other body parts. Other symptoms of pleural mesothelioma cancer include losing weight, severe breathing in trouble, fever, difficulty eating, and infection of the neck and face areas. It should be noted that some people with the disease will not experience any serious indications at all.