Imagine discovering that your liver, that unsung hero filtering toxins and powering your daily energy, is bogged down by excess fat. It’s a wake-up call, but here’s the hopeful part: fatty liver disease—now often called metabolic dysfunction-associated steatotic liver disease (MASLD)—isn’t a one-way street. With the right steps, many people can halt its progress, reduce fat buildup, and even reverse early damage. Affecting up to 25% of adults worldwide, this condition sneaks up on those with extra weight, diabetes, or high cholesterol, but it’s highly responsive to lifestyle changes. Drawing from the latest expert guidelines, let’s explore what to do if you’ve been diagnosed, backed by solid science and practical advice to get you started.
Understanding Your Diagnosis: It’s Not Too Late
Fatty liver happens when fat accumulates in liver cells, often without symptoms at first. There are two main types: simple fatty liver (steatosis), which is milder and reversible, and the more serious steatohepatitis (like NASH or MASH), where inflammation can lead to scarring, cirrhosis, or worse. The good news? Early detection through blood tests, ultrasounds, or FibroScan makes a huge difference. According to the American Association for the Study of Liver Diseases (AASLD) and the American Association of Clinical Endocrinology (AACE), most cases are tied to metabolic issues, not alcohol, and the key to management is tackling those root causes.
A 2023 review in The Lancet Gastroenterology & Hepatology highlights that lifestyle interventions can reduce liver fat by 30-50% in just months for many patients. But first things first: partner with your doctor. They might recommend monitoring with non-invasive tests like the Fibrosis-4 (FIB-4) score to check for advanced damage, avoiding unnecessary biopsies. If you have diabetes or heart risks, that’s priority number one—fatty liver amps up your chances of cardiovascular trouble by 64%, per AASLD data.
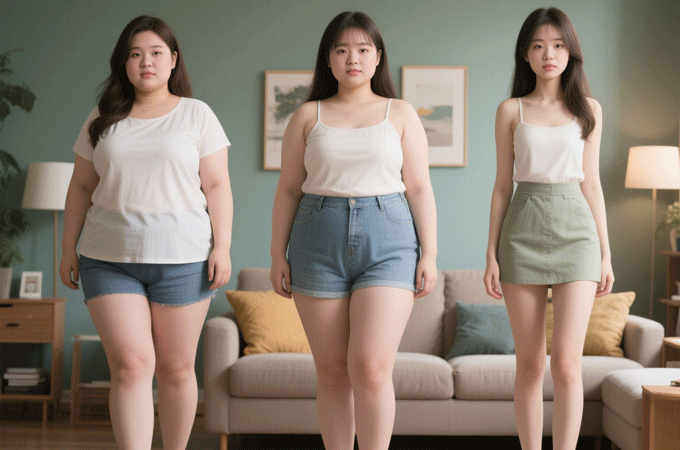
Step 1: Lose Weight the Smart Way—It’s Your Best Weapon
Weight loss is the cornerstone of fighting fatty liver, and it doesn’t have to be drastic to work. Aim for 7-10% of your body weight over 6-12 months; even 3-5% can cut liver fat significantly. A 2022 AACE guideline, co-sponsored by AASLD, reports that gradual loss through diet and exercise improves liver enzymes and reduces inflammation in up to 90% of cases.
Your User Guide to Sustainable Weight Loss:
Set Realistic Goals: Start with 1-2 pounds per week. Track progress with a journal or app, not just the scale—measure waist circumference too, as belly fat is a big culprit.
Diet Tweaks: Focus on a Mediterranean-style eating plan: plenty of veggies, fruits, whole grains, lean proteins (fish, poultry, beans), and healthy fats like olive oil and nuts. Cut back on sugary drinks, processed carbs, and fried foods—these spike insulin and pile on liver fat. A study in Hepatology (2018) showed this approach slashes steatosis by 40% in six months.
Portion Control: Use smaller plates and eat mindfully. Swap soda for water infused with lemon or berries.
Pro Tip: If you’re overweight, consider consulting a registered dietitian. Apps like MyFitnessPal can help log meals without overwhelming you.
Step 2: Get Moving—Exercise Without the Gym Dread
You don’t need to run marathons; consistent activity alone can drop liver fat by 20-30%, even without major weight loss. The European Association for the Study of the Liver (EASL) 2024 guidelines emphasize 150 minutes of moderate exercise weekly, mixing cardio and strength training to boost metabolism and insulin sensitivity.
A Beginner-Friendly Exercise Plan:
Start Slow: If you’re new to it, begin with 10-15 minute walks daily, building to brisk 30-minute sessions five days a week. Swimming or cycling are gentle on joints.
Build Strength: Add resistance exercises like bodyweight squats, light weights, or yoga twice weekly. Aim for 2-3 sets of 10-12 reps.
Make It Fun: Pair workouts with podcasts or walks with a friend. Track with a fitness tracker to stay motivated.
Evidence Check: A 2021 meta-analysis in Journal of Hepatology found aerobic exercise reduces liver stiffness (a sign of fibrosis) by 25% in NAFLD patients.
Step 3: Ditch the Vices and Fine-Tune Your Habits
Alcohol is a no-go— even moderate amounts can worsen damage, as per AASLD. Limit to zero if possible, especially if you have inflammation. Smoking? Quit it; it accelerates fibrosis. For medications, review everything with your doctor—some like steroids or tamoxifen can aggravate fatty liver.
Daily Habits for Liver Love:
Hydrate and Sleep: Drink 8-10 glasses of water daily and aim for 7-9 hours of sleep. Poor sleep disrupts metabolism, per a 2020 Nature Reviews study.
Manage Stress: Chronic worry raises cortisol, which promotes fat storage. Try meditation apps or deep breathing for 10 minutes a day.
Medications if Needed: No FDA-approved drug solely for fatty liver yet, but if you have diabetes, GLP-1 agonists like semaglutide (Wegovy) show promise in trials, reducing liver fat by 30-50% (AACE 2022). Pioglitazone might help NASH, but only under supervision. Vitamin E (800 IU/day) is sometimes recommended for non-diabetics with confirmed NASH, but discuss risks like prostate issues.
When to Seek Extra Help: Red Flags and Advanced Care
Most people manage fatty liver at home, but watch for fatigue, abdominal pain, jaundice, or swelling—these signal progression. If tests show fibrosis, you might need specialist care, like from a hepatologist. Bariatric surgery is an option for severe obesity, with studies showing 80% improvement in liver health post-procedure (AASLD).
Hope on the Horizon: You’re in Control
Fatty liver can feel overwhelming, but it’s one of the most reversible chronic conditions out there. By focusing on weight loss, exercise, and healthy habits, you’re not just protecting your liver—you’re boosting your heart health, energy, and overall vibe. Start small, celebrate wins, and lean on your healthcare team. Many folks see real changes in weeks, proving that a fatty liver diagnosis is more starting line than finish.
This article is informed by guidelines from the American Association for the Study of Liver Diseases (AASLD) and American Association of Clinical Endocrinology (AACE) on MASLD/NAFLD management, including the 2022 AACE Clinical Practice Guideline and 2024 EASL updates, alongside supporting research from Hepatology and Journal of Hepatology.